Nanomedicine has emerged as a promising field that utilizes the power of nanotechnology to revolutionize the treatment of various diseases. By harnessing the unique properties of nanoparticles, nanomedicine offers numerous advantages in the realm of blood disorders and transfusions. In this article, we will explore how nanomedicine is transforming the landscape of blood-related conditions and the potential benefits it brings.
The Significance of Nanomedicine in Blood Disorders
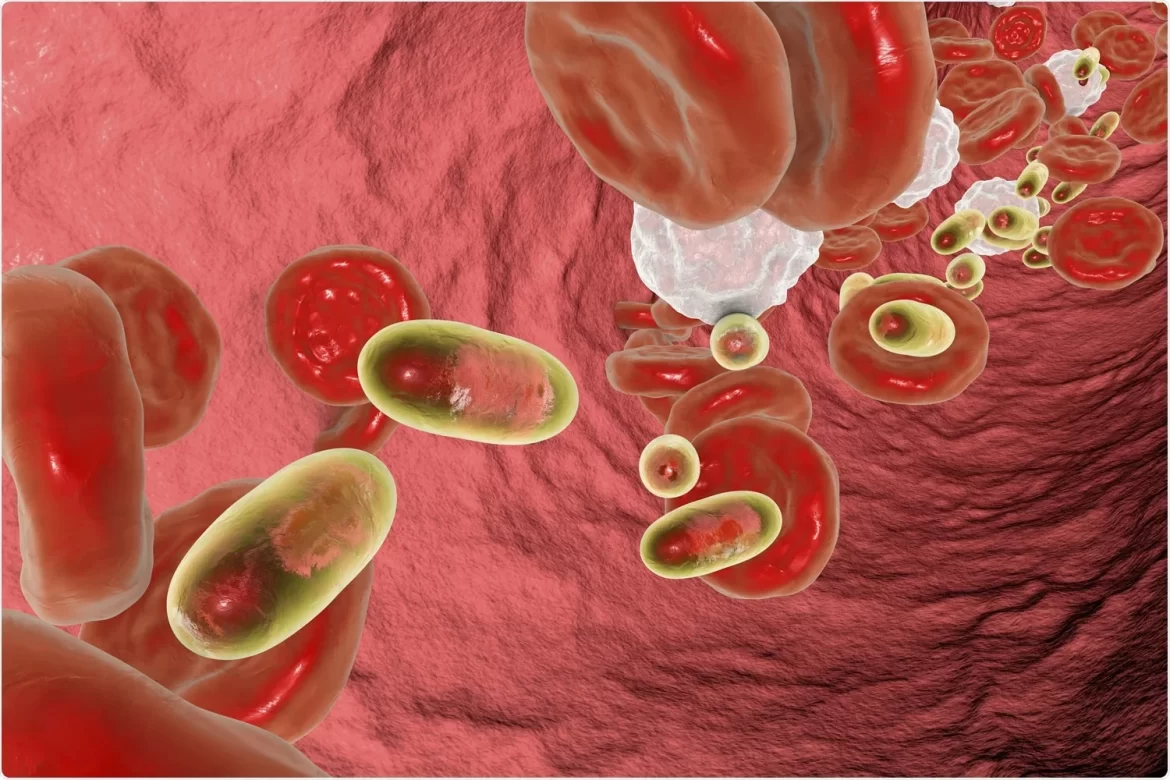
Understanding the Composition of Blood
Before delving into the nanomedicine advantages, it is essential to comprehend the composition of blood. Blood is a remarkable fluid connective tissue that plays a vital role in our overall health. It consists of two main components: the liquid part, called plasma, and the solid portion, which comprises red blood cells (RBCs), white blood cells (WBCs), and platelets.
Plasma, the liquid component, contains water, salts, minerals, nutrients, and proteins that facilitate various essential functions within the body. RBCs transport oxygen from the lungs to the tissues and carry carbon dioxide back to the lungs for elimination. WBCs, on the other hand, are circulating immune cells that constantly scan our blood and tissues to respond to pathogen invasions. Platelets are crucial in preventing and repairing vessel bleeding, as they play a key role in the process of hemostasis.
Blood Disorders and Their Impact
Blood disorders can significantly disrupt the normal functioning of the body and lead to various health complications. Conditions such as anemia, hemochromatosis, leukocytosis, and polycythemia vera can have debilitating effects on individuals. For instance, anemia, characterized by low levels of healthy RBCs, can cause fatigue, dyspnea, and cognitive dysfunction. Hemochromatosis, on the other hand, results in an excess of iron, leading to liver disease, heart problems, and diabetes. Leukocytosis and leukopenia involve an abnormal increase or decrease in WBCs, respectively, and can be associated with infections, autoimmune diseases, and various forms of cancer. Polycythemia vera, a rare blood cancer, is characterized by the excessive production of RBCs, WBCs, and platelets.
Advantages of Nanomedicine in Blood Disorders
Nanoparticles as Blood Substitutes
Blood transfusions have traditionally been a common therapeutic approach for blood disorders and severe hemorrhages. However, they come with significant limitations, including storage challenges, a lack of donors, compatibility issues, and the risk of complications for recipients. To overcome these limitations, the concept of Patient Blood Management (PBM) has been implemented, and researchers have explored the development of blood substitutes and plasma supplements.
Nanoparticles have shown great potential as blood substitutes, providing a viable alternative to traditional transfusions. These synthetic particles can mimic the functions of RBCs, WBCs, and platelets, offering numerous advantages. For instance, they can be stored for longer periods without refrigeration, reducing the storage challenges associated with traditional blood transfusions. Moreover, nanoparticles can be designed to be universally compatible, eliminating the need for matching blood types. By reducing the risk of adverse effects and complications, nanomedicine offers a safer and more efficient solution for patients with blood disorders.
Targeted Drug Delivery
One of the most significant advantages of nanomedicine in the treatment of blood disorders is its ability to deliver drugs directly to the affected tissues. Nanoparticles can be engineered to carry therapeutic agents, such as chemotherapy drugs, precisely to the desired target site, minimizing damage to healthy cells and improving treatment efficacy. This targeted drug delivery system ensures that the medication reaches its intended destination, enhancing the overall effectiveness of the treatment.
For example, in the treatment of cancer, nanomedicine has revolutionized chemotherapy by utilizing nanoparticles to deliver anti-cancer drugs specifically to tumor cells. By encapsulating the drugs within nanoparticles, they can bypass healthy cells and selectively target cancerous cells, reducing side effects and increasing treatment efficiency. This targeted approach minimizes toxicity to healthy tissues and improves the balance between efficacy and safety.
Improved Pharmacokinetics and Bioavailability
Nanoparticles offer improved pharmacokinetics and bioavailability, enhancing the therapeutic potential of drugs used in the treatment of blood disorders. These tiny particles can be designed to have optimal characteristics, such as controlled release, prolonged circulation time, and enhanced stability. By encapsulating drugs within nanoparticles, their degradation and clearance by the immune system can be minimized, leading to an extended half-life and enhanced efficacy.
Moreover, nanomedicine allows for the modulation of drug release kinetics, ensuring a sustained and controlled release of therapeutic agents. This sustained release can be particularly beneficial in cases where continuous drug delivery is required, such as in the treatment of chronic blood disorders or in post-operative care. By maintaining therapeutic drug levels over an extended period, nanomedicine provides a more consistent and effective treatment approach.
Camouflaging Nanoparticles for Enhanced Functionality
To further amplify the advantages of nanomedicine, researchers have explored the concept of “camouflaging” nanoparticles with the membranes of blood cells, such as RBCs and platelets. This approach aims to create “stealth” nanoparticles that can evade the immune system and enhance their functionality.
By coating nanoparticles with RBC or platelet membranes, researchers have successfully developed nanoparticles with improved biocompatibility and immune evasion properties. This camouflaging technique allows nanoparticles to mimic the surface properties of blood cells, making them less likely to be recognized as foreign entities by the immune system. This strategy not only enhances the safety and efficacy of nanomedicine but also opens up new possibilities for targeted drug delivery and personalized medicine.
Nanotechnology in Blood Transfusions
Overcoming Limitations of Traditional Transfusions
Nanotechnology offers innovative solutions to overcome the limitations associated with traditional blood transfusions. One of the major challenges of blood transfusions is the storage of blood, which must be refrigerated and used within a limited time frame.
Nanotechnology in blood substitutes can be engineered to have longer shelf lives, eliminating the need for constant refrigeration and reducing the wastage of valuable resources.
Moreover, nanotechnology enables the development of synthetic blood substitutes that are universally compatible with all blood types. This eliminates the need for blood type matching and expands the pool of potential donors, addressing the issue of donor shortages. With nanotechnology, blood transfusions can become more readily available, especially in critical situations where immediate access to compatible blood is crucial.
Synthetic Blood Substitutes
Nanotechnology has paved the way for the development of synthetic blood substitutes that can effectively mimic the functions of RBCs, WBCs, and platelets. These synthetic substitutes offer several advantages over traditional transfusions. For instance, they can be designed to have an extended shelf life, eliminating the urgency associated with using donated blood within a short timeframe. Furthermore, synthetic blood substitutes can be engineered to be universally compatible, eliminating the need for blood type matching and reducing the risk of adverse reactions.
Nanoparticles can also be used to encapsulate therapeutic agents, allowing for targeted drug delivery during transfusions. This enables the simultaneous administration of medications that can address underlying conditions or enhance the therapeutic effects of transfusions. By incorporating nanoparticles into synthetic blood substitutes, researchers have the opportunity to revolutionize the field of transfusion medicine, providing safer and more efficient treatment options for patients with blood disorders.
Current Innovations and Future Prospects
In recent years, significant advancements have been made in the field of nanomedicine, particularly in the context of blood disorders and transfusions. Researchers have explored various nanotechnological approaches, such as the development of nanocarriers for targeted drug delivery, the design of synthetic blood substitutes, and the use of camouflaged nanoparticles for enhanced functionality.
These innovations have shown promising results in preclinical and clinical studies, paving the way for future developments in nanomedicine. As nanotechnology continues to evolve, it holds the potential to revolutionize the treatment of blood disorders, offering improved therapeutic options, enhanced patient outcomes, and a reduced reliance on traditional transfusions.
In conclusion, nanomedicine provides a paradigm shift in the treatment of blood disorders and transfusions. With its numerous advantages, including targeted drug delivery, improved pharmacokinetics, and the development of synthetic blood substitutes, nanotechnology holds immense promise in improving patient care and outcomes. As researchers continue to push the boundaries of nanomedicine, we can expect to witness further breakthroughs and innovations that will transform the landscape of blood-related conditions and revolutionize the field of healthcare.